NEWS
News Conference - Lori Porter - Joplin, Missouri
Lori Porter, NAHCA CEO, on MSNBC
CNA Appreciation Week - KSN Coverage - April 2020
“The energy and the empowerment that NAHCA has given to our state has truly enhanced the depth of membership and the work that we do as a state association.”
“The energy and the empowerment that NAHCA has given to our state has truly enhanced the depth of membership and the work that we do as a state association.”
“The energy and the empowerment that NAHCA has given to our state has truly enhanced the depth of membership and the work that we do as a state association.”
“When you have satisfied and content CNAs, the care is better, and you’re going to have less nursing assistant turnover.”
NAHCA CNA
Print NEWS


An analysis of incomplete data shows they had a death rate higher than that of loggers, and may have rivaled fishers for most perilous profession
Feb. 18, 2021 – Scientific American – by Tanya Lewis

When you think of the most dangerous jobs in the U.S., you might imagine something like logging, fishing or truck driving. But in 2020 one of the deadliest professions of all did not involve operating heavy machinery, braving the elements or driving big rigs—but rather caring for the elderly.
When you think of the most dangerous jobs in the U.S., you might imagine something like logging, fishing or truck driving.
But in 2020 one of the deadliest professions of all did not involve operating heavy machinery, braving the elements or driving big rigs—but rather caring for the elderly.
As COVID-19 swept across the world last year, death rates among nursing home staff ranked among the highest for any job in the U.S., based on a Scientific American analysis of data from the Centers for Medicare & Medicaid Services (CMS) and the Bureau of Labor Statistics. But the CMS, which sets quality standards for skilled nursing facilities, only started requiring nursing homes to report such deaths in May 2020—just after last spring’s devastating peak in COVID deaths in parts of the country. So the calculated death rate is almost certainly an undercount, says Judith Chevalier, a Yale University professor of finance and economics who helped analyze the data.
The pandemic’s high toll among nursing home residents is well known, but the impact on staff has been far less visible. Workers in skilled nursing facilities had at least 80 deaths per 100,000 full-time employees last year. This estimate was calculated by dividing the total deaths among nursing home staff reported to the CMS from May 17 through December 27, 2020, by the total number of people who work at such facilities, as reported by the BLS. In comparison, fishers and related workers had 145 deaths per 100,000 people in 2019, according to data from the BLS. Loggers had 68.9 deaths per 100,000 people in the same year. Given that the CMS data for 2020 were only reported from last May onward, the full year’s actual death rate for nursing home staff may have approached or even exceeded that of fishers.
Inside nursing homes, certified nursing assistants, or CNAs, perform some of the most important—and often thankless—work. It can include feeding nursing home residents, bathing them and turning them over so they do not get bedsores. Yet many of these workers are paid minimum wage and often have little or no sick leave, says Lori Porter, co-founder and chief executive officer of the National Association of Health Care Assistants, an organization that represents CNAs. Additionally, nursing homes were chronically understaffed and underfunded even before the pandemic. So when COVID hit, many of them were vastly unprepared. They lacked personal protective equipment (PPE), adequate infectious disease training, access to frequent testing and backup staff to cover for sick employees. As a result, these facilities have been among the communities hit hardest by the pandemic.
“If COVID has had a positive [effect] on anything, it’s that it’s no longer nursing homes’ dirty little secret—it’s America’s—that we don’t take care of our old people,” Porter says. “That’s the real story…. Why are we warehousing our old people in human filing cabinets?”
Last summer Porter, a former CNA herself, served on the Coronavirus Commission on Safety and Quality in Nursing Homes … (read more)

Feb. 1, 2021 – Skilled Nursing News – by Maggie Flynn
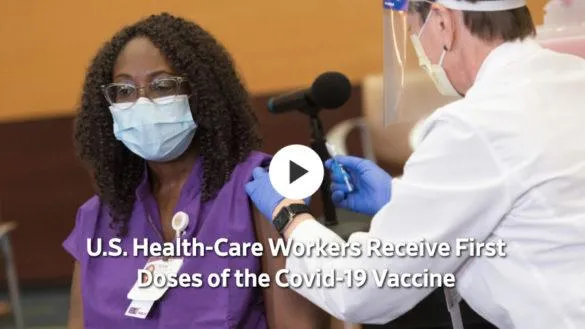
When the effort to vaccinate long-term care workers and residents began to gather momentum, hesitancy among workers became a prominent issue well before the first shots were administered.
The issue of whether or not workers — burned out by the ongoing tragedy of resident and staff deaths from COVID-19, personal protective equipment (PPE) shortages, and ongoing slow or bungled responses to the crisis by both federal and state governments — would trust the institutions now telling them to take a vaccine came up in December, shortly before the first COVID-19 vaccine received its emergency use authorization (EUA).
Touchstone Communities, which is based in San Antonio and has 28 skilled nursing facilities in the state of Texas, saw the ebb and flow of emotions around the vaccine play out even before the EUA was granted. When news of progress on the vaccines began to trickle out over the course of the summer of 2020, the initial reaction of staff members was quite optimistic, Touchstone COO Leslie Cunningham Campbell told Skilled Nursing News in an interview on January 25…
…“My concern is not necessarily the vaccine, if it’s proven safe,” Lori Porter, the CEO and co-founder of the National Association of Health Care Assistants (NAHCA), told SNN on December 2. “My fear is that if we don’t educate them, if we allow the facilities to provide the education on the vaccine, there is a trust issue. CNAs do not trust their leaders.”
On February 1, the CDC released a Morbidity and Mortality Weekly Report (MMWR) that confirmed a wide disparity in vaccine uptake between residents and staff. Out of 11,460 SNFs with at least one vaccination clinic conducted during the first month of the CDC’s Pharmacy Partnership for Long-Term Care Program, a median of 77.8% of residents had at least one dose — compared with a median of 37.5% of staff members. … (read more)

Jan. 27, 2021 – McKnight’s Long-Term Care News – by Danielle Brown
COVID-19 is now responsible for the deaths of more than 100,000 residents and staff in the 15,000 nursing homes in this country. I’ve been in this field 40 years —as a certified nursing assistant, an administrator, company executive and now as head of NAHCA — and I have never seen so many CNAs feel as helpless, hopeless and terrified as they have been since March.
Yet, here we are in the third wave of this invisible enemy, and CNAs are STILL in the same position they were in back then. They still feel helpless, hopeless and terrified. What is different now is that many more of them are dead or sick from COVID-19. Many have left their jobs in fear of getting the virus or in frustration from not having enough PPE to protect them. Some have been forced to use up their sick-time or other leave because of quarantine requirements after an exposure, and many more are still making an average of $13 per hour but caring for more residents on their shifts than they were pre-pandemic.
As I write, one of my board members — a CNA at the same nursing home for the last 25 years — lies in her bed at home, gravely ill with COVID-19 and without pay. Before she fell ill, she had already used her paid leave due to quarantine requirements, and now she must bear the brunt of the expense of this savage virus because she cared so deeply for the elders she serves. She is paid so little that she cannot afford insurance. The media has tried to cover this crisis with some objectivity, but many outlets have placed blame at the hands of nursing home owners and operators, which is where it truly does not belong. The root of the problem is an ageist and outdated system of care that does not value elders nor the people who care for them.
Nowhere is this more evident than in the measly Medicaid rates that Centers for Medicare & Medicaid Services and state governments pay to reimburse nursing homes.
Lori Porter is the CEO of the National Association of Health Care Assistants. She started her career as a CNA and later became a licensed nursing home administrator and regional operations director for 10 skilled nursing centers before co-founding NAHCA. Porter is the author of “Everything I Learned in Life I Learned in Long Term Care” and served on the 2020 White House Task Force’s Coronavirus Commission on Safety and Quality in Nursing Homes. … (read more)

Jan. 27, 2021 – McKnight’s Long-Term Care News – by Danielle Brown
New pandemic guidance on healthcare workplace safety could provide more clarity for providers and workers in long-term care, according to a leading expert.
President Joe Biden late last week signed an executive order directing the Occupational Safety and Health Administration to issue revised guidance to employers on workplace safety during the COVID-19 pandemic. The order calls on the agency to issue the revisions to employers within the next two weeks and to consider whether any emergency temporary standards are necessary.

Workers in long-term care, particularly certified nursing assistants, are one board with the move, according to Lori Porter, co-founder and CEO of the National Association of Health Care Assistants.
“CNAs, on the whole, would welcome anything that would create an atmosphere for the protection of themselves against the spread of COVID-19,” Porter told McKnight’s Long-Term Care News on Tuesday.
Porter explained that current guidance doesn’t address possible provider penalties. She noted that it also doesn’t account for how different long-term care is from other types of healthcare industries.
“One of the things that will be interesting is the staffing ratios, in terms of will they take into account the resident-to-certified nursing assistant staffing ratio as it pertains to workplace safety and health and safety?” she said. “That is what will remain to be seen.”
Porter stated that unclear sufficient staffing ratio measures from the federal level swats at potential solutions to address the issue. She said “that will likely have to be defined if it’s really going to be applicable to OSHA and skilled nursing.” … (read more)

Jan. 24, 2021 – Skilled Nursing News – by Alex Spanko
After the physical health and safety of residents and workers, the prospect of normal visitation looms as the top promise of a smooth rollout of COVID-19 vaccines to the nation’s nursing homes. But operators will likely not make any moves until they’re given the all-clear by state and federal regulators, with a significant percentage planning to require vaccinations for all visitors before reopening their doors to family and friends. Just about half of respondents to a recent online Skilled Nursing News poll said they would mandate proof of vaccination for potential visitors, while a nearly equal number said they would not.
The relative lack of enthusiasm among frontline caregivers to receive the vaccine has been the primary story of the mass inoculation effort so far. Even before the Food and Drug Administration (FDA) granted emergency authorization to the Pfizer and Moderna shots in December, leaders sounded the alarm about the deep skepticism they were hearing among rank-and-file nursing home employees.
Touchstone Communities, which is based in San Antonio and has 28 skilled nursing facilities in the state of Texas, saw the ebb and flow of emotions around the vaccine play out even before the EUA was granted. When news of progress on the vaccines began to trickle out over the course of the summer of 2020, the initial reaction of staff members was quite optimistic, Touchstone COO Leslie Cunningham Campbell told Skilled Nursing News in an interview on January 25…
Lori Porter, CEO and co-founder of the National Association of Health Care Assistants (NAHCA), framed it as a matter of trust in a December interview with SNN: After having watched their residents and coworkers die over the past year, while also struggling with shortages of personal protective equipment (PPE) and constant worries about their own physical and mental health, many nursing home workers have lost faith in the institutions now telling them that the vaccines are safe and necessary.
“My concern is not necessarily the vaccine, if it’s proven safe,” Porter told SNN. “My fear is that if we don’t educate them, if we allow the facilities to provide the education on the vaccine, there is a trust issue. CNAs do not trust their leaders.” … (read more)

Some staff in hospitals and long-term care facilities don’t want to take the Covid-19 vaccine. Their employers are trying to change their minds.
Jan. 14, 2021 – The New York Times – by Rebecca Robbins, Sabrina Tavernise and Sharon Otterman
Anxious about taking a new vaccine and scarred by a history of being mistreated, many frontline workers at hospitals and nursing homes are balking at getting inoculated against Covid-19. Anxious about their patients’ health and scarred by many thousands of deaths in the past year, hospitals and nursing homes are desperate to have their employees vaccinated.
Those opposing forces have spawned an unusual situation: In addition to educating their workers about the benefits of the Covid-19 vaccines, a growing number of employers are dangling incentives like cash, extra time off and even Waffle House gift cards for those who get inoculated, while in at least a few cases saying they will fire those who refuse. Officials at two large long-term care chains, Juniper Communities and Atria Senior Living, said they were requiring their workers, with limited exceptions, to take the vaccine if they wanted to keep their jobs.
Another concern about forcing workers to get vaccinated is that it could prompt hesitant employees to resign. That’s a particular worry in long-term care, where the pandemic has exacerbated a shortage of certified nursing assistants.
“We’re having a hard time filling those roles and those positions now, and if we lose more people, then our old people are going to suffer,” said Dane Henning, Director of Public Affairs at the National Association of Health Care Assistants. … (read more)

Expert insights on how the industry should evolve in response to CO
Jan. 13, 2021 – AARP – by Sari Harrar, Joe Eaton and Harris Meyer

It’s complicated. This phrase has become the default and arguably lazy response to many 21st-century challenges. But when it comes to finding ways to reform and improve America’s nursing homes, it is sadly accurate.
The roots of the long-term care industry’s problems are deeply tangled, as we reported in the December issue of the AARP Bulletin.
…A nursing home aide can be responsible for more than 20 residents on a shift. The job is physically and emotionally demanding, and lives can be at stake, yet the average wage is around $13 an hour. Requirements for the job vary by state. In most, workers complete a hands-on training course and a certified nursing assistant (CNA) program, which generally take from 75 hours of training to more than three months. But don’t be fooled by the terminology. State requirements to gain a hairstylist license are more demanding than for a CNA, says Lori Porter, cofounder and CEO of the National Association of Health Care Assistants. Now that COVID-19 restrictions have limited CNAs to working at just one facility, many are unable to afford basic living expenses. … (read more)

Jan. 10, 2021 – Skilled Nursing News – by Alex Spanko
If there’s been one recurring theme for SNN’s annual executive outlook, it’s the idea that putting 2020 to bed represents a chance to reset and move on past the worst year in the history of the post-acute and long-term space, both in the United States and around the world.
But that can only happen if the public and the frontline workers who serve our seniors believe that change is possible — and forthcoming.
The stories of admission declines and vaccine hesitancy among caregivers prove that trust in nursing homes has never been lower, and that coming back from a world-historic disaster won’t be a simple matter of flipping over a calendar page.
Lori Porter, CEO, National Association of Health Care Assistants
I — along with many, many others — am happy to see the year 2021 and have 2020 in the rearview. The last year was incredibly difficult on everyone, especially those in our field. The pandemic has been on a rampage through America’s nursing homes, wreaking havoc on our elders. However, the new year signifies a new beginning, a fresh start, and new opportunities. New opportunities often come with new challenges.
As co-founder and CEO of the association of and for certified nursing assistants (CNAs), my focus is lasered in on the front line. What was once a generally safe profession is now one of the most dangerous in America due to the pandemic. … (read more)

Jan. 5, 2021 – Skilled Nursing News – by Alex Spanko
Only about 13% of the first COVID-19 vaccine doses have been administered to nursing home residents by the first business week of 2021, raising concerns about the rollout for both the elderly and the general public.
The federal government’s long-term care vaccination initiative has about 3.3 million total doses set aside, but just 429,066 had been administered in the setting as of January 5, according to the most recent data from the Centers for Disease Control & Prevention (CDC); the latter figure represents just the first dose in the two-stage vaccination process. Around 17 million vaccine doses have been distributed nationwide, with about 4.8 million first rounds injected thus far, the CDC reported…
…Operators are also beginning to face predicted resistance to the vaccine among nursing home staff, who have spent the last 10 months on the front lines of a crisis that has shown no signs of abating. In Ohio, for instance, up to 60% of workers declined the vaccine, Gov. Mike DeWine indicated last week, despite more widespread acceptance among residents.
Lori Porter, CEO and co-founder of the National Association of Health Care Assistants, said last month that many of the certified nursing assistants (CNAs) that her organization represents have lost faith in institutions — including the government and their employers — after witnessing firsthand the COVID-19 disaster in long-term care.
“My concern is not necessarily the vaccine, if it’s proven safe,” Porter told SNN. “My fear is that if we don’t educate them, if we allow the facilities to provide the education on the vaccine, there is a trust issue. CNAs do not trust their leaders.” … (read more)

Dec. 30, 2020 – Washington Post – by Isaac Stanley-Becker

In suburban Milwaukee, clinicians recently discarded 500 doses of coronavirus vaccine after vials were “intentionally” left unrefrigerated. In southeastern Arizona, a rural clinic has enough shots but too few employees lining up to take them. And on the coast of Maine, physicians have been left in the dark about when they will get vaccinated.
The largest immunization campaign in U.S. history is off to a slow start, dimming hopes, at the end of a dismal year, of an imminent return to normal. physicians have been left in the dark about when they will get vaccinated.
In some places, the vaccination campaign — among the most complex logistical efforts initiated in peacetime — has been marked by chaos and confusion. Many medical workers who believe they should have priority access are finding that inoculation remains elusive. And most states moved into the third week of immunization not yet beginning to get shots to long-term care facilities, which have been epicenters of infection……But hesitancy among nursing home staffers looms as a significant hurdle. Lori Porter, who leads the National Association of Health Care Assistants, said polling she has reviewed suggests a significant majority of people working in stricken facilities “are a hard no” on taking the vaccine. “Often, people have to see something before they can believe something, especially in this political climate,” she said, predicting at least moderate improvement as immunization becomes a reality across the country. … (read more)

Dec. 22, 2020 – Skilled Nursing News – by Maggie Flynn
With two COVID-19 vaccines officially authorized for use, the immunization of health care workers and long-term care facility residents is finally underway in earnest. The Food and Drug Administration granted emergency use authorizations (EUAs) to Pfizer’s (NYSE: PFE) COVID-19 vaccine on December 11 and to Moderna’s (Nasdaq: MRNA) on December 18 . There are several considerations for skilled nursing facilities to take into account as they prepare for the inoculations, from how to handle staff concerns about taking the vaccine to preparing for the impact side effects could have on scheduling.
Vaccinating staff is the critical first step for facilities, from which all the other considerations about workflow and coordination will spring. A webinar held on December 17 tackled some of those considerations. Hosted by the National Association of Health Care Assistants (NAHCA) and AMDA – The Society for Post-Acute and Long-Term Care Medicine, the virtual event gave an overview of some of the concerns expressed by certified nursing assistants (CNAs), with questions and answers between frontline staff and long-term care physicians.
Ultimately, long-term care workers will not be forced to take COVID-19 vaccines, webinar speakers said, even though an advisory committee for the CDC recommended that health care workers and long-term care residents be first in line . “I’m not going to get up here and tell you that ‘You have got to take the shot, get the vaccine,’” Lori Porter, the CEO and co-founder of NAHC , said during the webinar. “That is a choice you will have to make yourself.” … ( read more )

Dec. 22, 2020 – Skilled Nursing News – by Maggie Flynn
With two COVID-19 vaccines officially authorized for use, the immunization of health care workers and long-term care facility residents is finally underway in earnest. The Food and Drug Administration granted emergency use authorizations (EUAs) to Pfizer’s (NYSE: PFE) COVID-19 vaccine on December 11 and to Moderna’s (Nasdaq: MRNA) on December 18.
There are several considerations for skilled nursing facilities to take into account as they prepare for the inoculations, from how to handle staff concerns about taking the vaccine to preparing for the impact side effects could have on scheduling.
Vaccinating staff is the critical first step for facilities, from which all the other considerations about workflow and coordination will spring. A webinar held on December 17 tackled some of those considerations. Hosted by the National Association of Health Care Assistants (NAHCA) and AMDA – The Society for Post-Acute and Long-Term Care Medicine, the virtual event gave an overview of some of the concerns expressed by certified nursing assistants (CNAs), with questions and answers between frontline staff and long-term care physicians.
Ultimately, long-term care workers will not be forced to take COVID-19 vaccines, webinar speakers said, even though an advisory committee for the CDC recommended that health care workers and long-term care residents be first in line. “I’m not going to get up here and tell you that ‘You have got to take the shot, get the vaccine,’” Lori Porter, the CEO and co-founder of NAHCA, said during the webinar. “That is a choice you will have to make yourself.” … (read more)

Dec. 17, 2020 – Barrons.com – by Eleanor Laise

Sherry Perry has seen all the horrors of the pandemic. As a certified nursing assistant at a long-term care facility in Lebanon, Tenn., she has held a phone up to a window so a daughter could say goodbye to her dying father. She has watched residents die alone, not understanding why their families didn’t visit them in their final days. Earlier this month, she herself got Covid, suffering fever and chills, and passing out as she struggled to breathe.
As the Covid-19 vaccine arrives in long-term care facilities this month, however, Perry, who is also a board member of the National Association of Health Care Assistants (NAHCA), says she and many of her co-workers are concerned about side effects and distrustful of the government.
As the Covid-19 vaccine arrives in long-term care facilities this month, however, Perry, who is also a board member of the National Association of Health Care Assistants (NAHCA), says she and many of her co-workers are concerned about side effects and distrustful of the government. With a maximum of six paid sick days a year, she fears having to take unpaid time off. Her facility hasn’t told staff anything about the vaccine’s arrival, she says, and “that throws people into panic mode,” because they fear they’ll be pushed into taking a brand-new vaccine that they don’t fully understand.. … (read more)

Dec. 16, 2020 – The New York Times – by Rebecca Robbins and Jessica Silver-Greenberg
It promises to be a crucial milestone in America’s battle against a pandemic that has inflicted especially severe carnage on nursing homes. At least 106,000 residents and staff of long-term care facilities have died from the virus, accounting for 38 percent of the country’s Covid-related fatalities.
But even before it begins, the mass-vaccination campaign is facing serious obstacles that are worrying nursing home executives, industry watchdogs, elder-care lawyers and medical experts. They expect nursing homes to be the most challenging front in the mission to vaccinate Americans…
…“I don’t want to be a guinea pig,” said Sheena Bumpas, a certified nursing assistant at a home in Duncan, Okla. She is far from alone. When the National Association of Health Care Assistants, an advocacy group for caregivers, recently surveyed certified nursing assistants who work in long-term care facilities, nearly 72 percent of respondents said they do not want to receive the vaccine.
Lori Porter, the group’s co-founder and chief executive, said employees are also worried about what happens if they experience side effects — some participants in clinical trials experienced mild to moderate side effects — that force them to stay home. Ms. Porter said many nursing assistants had to use sick days to quarantine earlier in the pandemic and now have little or no paid sick leave left for 2020. … (read more)

100,000 COVID Dead in Long-Term Care?
Dec. 3, 2020 – AARP.org

To understand who or what is to blame for the more than 100,000 deaths caused by the coronavirus among residents and staff of U.S. long-term care facilities between March and Thanksgiving, it’s useful to consider a devastating calamity that hit in 2005: Hurricane Katrina.
In the days, weeks and months after New Orleans was overwhelmed with flooding from the hurricane, critics pointed to the slow response from the federal government, decisions made by the city’s mayor and the state’s governor, a delay in engagement from the U.S. president, the greed and influence of private businesses, and even the stubbornness of the city’s residents as the causes for all the pain that had occurred.
some level of truth. But in time, two simple but profound causes were ultimately found to be the root of what happened: bad infrastructure decisions that dated back decades—in New Orleans’ case, a poorly maintained, inadequate levee system — and a storm of such magnitude that once 23 of the levees were breached, little could be done to prevent 80 percent of the city from going underwater…
…In July, a report published by the National Bureau of Economic Research raised alarms about the common practice of care staff working in multiple facilities. Nursing homes with higher rates of shared staffing, the researchers found, had higher rates of infection. Limiting care staff to a single nursing home, they concluded, could reduce COVID-19 infections in facilities by 44 percent.
That’s no surprise to Lori Porter, cofounder of the National Association of Health Care Assistants, which represents many nursing home care workers. With an average wage of around $13 an hour, care workers often work at multiple nursing homes to make ends meet, Porter says. Many staffers don’t receive health insurance or paid sick leave, leading some to work even when they were experiencing coronavirus-type symptoms. “What did you think was going to happen?” Porter says. … (read more)

Dec. 2, 2020 – Skilled Nursing News – by Maggie Flynn
The Centers for Disease Control and Prevention (CDC) was emphatic in a Tuesday meeting that it has the systems and processes in place to keep track of any adverse events from a COVID-19 vaccine, whenever one is approved.
Whether that is enough to quell the concerns of the health care workers and long-term care facility residents — whom the CDC’s Advisory Committee on Immunization Practices (ACIP) this week recommended should be first in line for immunization — is still an open question.
“There is hesitancy, of course,” Lori Porter, the CEO and co-founder of the National Association of Health Care Assistants (NAHCA), told Skilled Nursing News on December 2. “Until we know if it’s mandated or not, we’re not really going to know exactly what’s going to happen. From what we can tell, the CDC won’t make it mandatory. It’ll be up to the states, and the states might pass it off to the facilities as more of an employer policy. So until we know what the outcome is, there is a great deal of hesitancy among CNAs [certified nursing assistants].” … (read more)

Oct. 18, 2020 – Senior Living Foresight – by Steve Moran

Hands-heartIn response to COVID-19 and the disastrous impact it has had on nursing homes, the president established an independent body called the Coronavirus Commission on Safety and Quality in Nursing Homes. One of the members of the commission was Lori Porter the CEO of the National Association of Health Care Assistants.
some level of truth. But in time, two simple but profound causes were ultimately found to be the root of what happened: bad infrastructure decisions that dated back decades—in New Orleans’ case, a poorly maintained, inadequate levee system — and a storm of such magnitude that once 23 of the levees were breached, little could be done to prevent 80 percent of the city from going underwater…
…In July, a report published by the National Bureau of Economic Research raised alarms about the common practice of care staff working in multiple facilities. Nursing homes with higher rates of shared staffing, the researchers found, had higher rates of infection. Limiting care staff to a single nursing home, they concluded, could reduce COVID-19 infections in facilities by 44 percent.
That’s no surprise to Lori Porter, cofounder of the National Association of Health Care Assistants, which represents many nursing home care workers. With an average wage of around $13 an hour, care workers often work at multiple nursing homes to make ends meet, Porter says. Many staffers don’t receive health insurance or paid sick leave, leading some to work even when they were experiencing coronavirus-type symptoms. “What did you think was going to happen?” Porter says. … (read more)
Member Login
Virtual Campus Login
Job Board
CNA TV
Blog
Privacy
Terms
Your Benefits
as a NAHCA CNA Member


Nursing Home Workers
Had One of the Deadliest Jobs of 2020
An analysis of incomplete data shows they had a death rate higher than that of loggers, and may have rivaled fishers for most perilous profession
Feb. 18, 2021 – Scientific American – by Tanya Lewis

When you think of the most dangerous jobs in the U.S., you might imagine something like logging, fishing or truck driving. But in 2020 one of the deadliest professions of all did not involve operating heavy machinery, braving the elements or driving big rigs—but rather caring for the elderly.
When you think of the most dangerous jobs in the U.S., you might imagine something like logging, fishing or truck driving.
But in 2020 one of the deadliest professions of all did not involve operating heavy machinery, braving the elements or driving big rigs—but rather caring for the elderly.
As COVID-19 swept across the world last year, death rates among nursing home staff ranked among the highest for any job in the U.S., based on a Scientific American analysis of data from the Centers for Medicare & Medicaid Services (CMS) and the Bureau of Labor Statistics. But the CMS, which sets quality standards for skilled nursing facilities, only started requiring nursing homes to report such deaths in May 2020—just after last spring’s devastating peak in COVID deaths in parts of the country. So the calculated death rate is almost certainly an undercount, says Judith Chevalier, a Yale University professor of finance and economics who helped analyze the data.
The pandemic’s high toll among nursing home residents is well known, but the impact on staff has been far less visible. Workers in skilled nursing facilities had at least 80 deaths per 100,000 full-time employees last year. This estimate was calculated by dividing the total deaths among nursing home staff reported to the CMS from May 17 through December 27, 2020, by the total number of people who work at such facilities, as reported by the BLS. In comparison, fishers and related workers had 145 deaths per 100,000 people in 2019, according to data from the BLS. Loggers had 68.9 deaths per 100,000 people in the same year. Given that the CMS data for 2020 were only reported from last May onward, the full year’s actual death rate for nursing home staff may have approached or even exceeded that of fishers.
Inside nursing homes, certified nursing assistants, or CNAs, perform some of the most important—and often thankless—work. It can include feeding nursing home residents, bathing them and turning them over so they do not get bedsores. Yet many of these workers are paid minimum wage and often have little or no sick leave, says Lori Porter, co-founder and chief executive officer of the National Association of Health Care Assistants, an organization that represents CNAs. Additionally, nursing homes were chronically understaffed and underfunded even before the pandemic. So when COVID hit, many of them were vastly unprepared. They lacked personal protective equipment (PPE), adequate infectious disease training, access to frequent testing and backup staff to cover for sick employees. As a result, these facilities have been among the communities hit hardest by the pandemic.
“If COVID has had a positive [effect] on anything, it’s that it’s no longer nursing homes’ dirty little secret—it’s America’s—that we don’t take care of our old people,” Porter says. “That’s the real story…. Why are we warehousing our old people in human filing cabinets?”
Last summer Porter, a former CNA herself, served on the Coronavirus Commission on Safety and Quality in Nursing Homes … (read more)

Revised COVID-19 guidance from
OSHA coming under executive order
Feb. 1, 2021 – Skilled Nursing News – by Maggie Flynn
When the effort to vaccinate long-term care workers and residents began to gather momentum, hesitancy among workers became a prominent issue well before the first shots were administered.
The issue of whether or not workers — burned out by the ongoing tragedy of resident and staff deaths from COVID-19, personal protective equipment (PPE) shortages, and ongoing slow or bungled responses to the crisis by both federal and state governments — would trust the institutions now telling them to take a vaccine came up in December, shortly before the first COVID-19 vaccine received its emergency use authorization (EUA).
Touchstone Communities, which is based in San Antonio and has 28 skilled nursing facilities in the state of Texas, saw the ebb and flow of emotions around the vaccine play out even before the EUA was granted. When news of progress on the vaccines began to trickle out over the course of the summer of 2020, the initial reaction of staff members was quite optimistic, Touchstone COO Leslie Cunningham Campbell told Skilled Nursing News in an interview on January 25…
…“My concern is not necessarily the vaccine, if it’s proven safe,” Lori Porter, the CEO and co-founder of the National Association of Health Care Assistants (NAHCA), told SNN on December 2. “My fear is that if we don’t educate them, if we allow the facilities to provide the education on the vaccine, there is a trust issue. CNAs do not trust their leaders.”
On February 1, the CDC released a Morbidity and Mortality Weekly Report (MMWR) that confirmed a wide disparity in vaccine uptake between residents and staff. Out of 11,460 SNFs with at least one vaccination clinic conducted during the first month of the CDC’s Pharmacy Partnership for Long-Term Care Program, a median of 77.8% of residents had at least one dose — compared with a median of 37.5% of staff members. … (read more)

CNA WORKFORCE
at a breaking point
Jan. 27, 2021 – McKnight’s Long-Term Care News – by Danielle Brown
COVID-19 is now responsible for the deaths of more than 100,000 residents and staff in the 15,000 nursing homes in this country. I’ve been in this field 40 years —as a certified nursing assistant, an administrator, company executive and now as head of NAHCA — and I have never seen so many CNAs feel as helpless, hopeless and terrified as they have been since March.
Yet, here we are in the third wave of this invisible enemy, and CNAs are STILL in the same position they were in back then. They still feel helpless, hopeless and terrified. What is different now is that many more of them are dead or sick from COVID-19. Many have left their jobs in fear of getting the virus or in frustration from not having enough PPE to protect them. Some have been forced to use up their sick-time or other leave because of quarantine requirements after an exposure, and many more are still making an average of $13 per hour but caring for more residents on their shifts than they were pre-pandemic.
As I write, one of my board members — a CNA at the same nursing home for the last 25 years — lies in her bed at home, gravely ill with COVID-19 and without pay. Before she fell ill, she had already used her paid leave due to quarantine requirements, and now she must bear the brunt of the expense of this savage virus because she cared so deeply for the elders she serves. She is paid so little that she cannot afford insurance. The media has tried to cover this crisis with some objectivity, but many outlets have placed blame at the hands of nursing home owners and operators, which is where it truly does not belong. The root of the problem is an ageist and outdated system of care that does not value elders nor the people who care for them.
Nowhere is this more evident than in the measly Medicaid rates that Centers for Medicare & Medicaid Services and state governments pay to reimburse nursing homes.
Lori Porter is the CEO of the National Association of Health Care Assistants. She started her career as a CNA and later became a licensed nursing home administrator and regional operations director for 10 skilled nursing centers before co-founding NAHCA. Porter is the author of “Everything I Learned in Life I Learned in Long Term Care” and served on the 2020 White House Task Force’s Coronavirus Commission on Safety and Quality in Nursing Homes. … (read more)

Revised COVID-19 guidance from
OSHA coming under executive order
Jan. 27, 2021 – McKnight’s Long-Term Care News – by Danielle Brown
New pandemic guidance on healthcare workplace safety could provide more clarity for providers and workers in long-term care, according to a leading expert.
President Joe Biden late last week signed an executive order directing the Occupational Safety and Health Administration to issue revised guidance to employers on workplace safety during the COVID-19 pandemic. The order calls on the agency to issue the revisions to employers within the next two weeks and to consider whether any emergency temporary standards are necessary.

Workers in long-term care, particularly certified nursing assistants, are one board with the move, according to Lori Porter, co-founder and CEO of the National Association of Health Care Assistants.
“CNAs, on the whole, would welcome anything that would create an atmosphere for the protection of themselves against the spread of COVID-19,” Porter told McKnight’s Long-Term Care News on Tuesday.
Porter explained that current guidance doesn’t address possible provider penalties. She noted that it also doesn’t account for how different long-term care is from other types of healthcare industries.
“One of the things that will be interesting is the staffing ratios, in terms of will they take into account the resident-to-certified nursing assistant staffing ratio as it pertains to workplace safety and health and safety?” she said. “That is what will remain to be seen.”
Porter stated that unclear sufficient staffing ratio measures from the federal level swats at potential solutions to address the issue. She said “that will likely have to be defined if it’s really going to be applicable to OSHA and skilled nursing.” … (read more)

Nursing Home Providers Split
on Post-Vaccine Visitation Plans
Jan. 24, 2021 – Skilled Nursing News – by Alex Spanko
After the physical health and safety of residents and workers, the prospect of normal visitation looms as the top promise of a smooth rollout of COVID-19 vaccines to the nation’s nursing homes. But operators will likely not make any moves until they’re given the all-clear by state and federal regulators, with a significant percentage planning to require vaccinations for all visitors before reopening their doors to family and friends. Just about half of respondents to a recent online Skilled Nursing News poll said they would mandate proof of vaccination for potential visitors, while a nearly equal number said they would not.
The relative lack of enthusiasm among frontline caregivers to receive the vaccine has been the primary story of the mass inoculation effort so far. Even before the Food and Drug Administration (FDA) granted emergency authorization to the Pfizer and Moderna shots in December, leaders sounded the alarm about the deep skepticism they were hearing among rank-and-file nursing home employees.
Touchstone Communities, which is based in San Antonio and has 28 skilled nursing facilities in the state of Texas, saw the ebb and flow of emotions around the vaccine play out even before the EUA was granted. When news of progress on the vaccines began to trickle out over the course of the summer of 2020, the initial reaction of staff members was quite optimistic, Touchstone COO Leslie Cunningham Campbell told Skilled Nursing News in an interview on January 25…
Lori Porter, CEO and co-founder of the National Association of Health Care Assistants (NAHCA), framed it as a matter of trust in a December interview with SNN: After having watched their residents and coworkers die over the past year, while also struggling with shortages of personal protective equipment (PPE) and constant worries about their own physical and mental health, many nursing home workers have lost faith in the institutions now telling them that the vaccines are safe and necessary.
“My concern is not necessarily the vaccine, if it’s proven safe,” Porter told SNN. “My fear is that if we don’t educate them, if we allow the facilities to provide the education on the vaccine, there is a trust issue. CNAs do not trust their leaders.” … (read more)

Cash, Breakfasts and Firings:
An All-Out Push to Vaccinate Wary Medical Workers
Some staff in hospitals and long-term care facilities don’t want to take the Covid-19 vaccine. Their employers are trying to change their minds.
Jan. 14, 2021 – The New York Times – by Rebecca Robbins, Sabrina Tavernise and Sharon Otterman
Anxious about taking a new vaccine and scarred by a history of being mistreated, many frontline workers at hospitals and nursing homes are balking at getting inoculated against Covid-19. Anxious about their patients’ health and scarred by many thousands of deaths in the past year, hospitals and nursing homes are desperate to have their employees vaccinated.
Those opposing forces have spawned an unusual situation: In addition to educating their workers about the benefits of the Covid-19 vaccines, a growing number of employers are dangling incentives like cash, extra time off and even Waffle House gift cards for those who get inoculated, while in at least a few cases saying they will fire those who refuse. Officials at two large long-term care chains, Juniper Communities and Atria Senior Living, said they were requiring their workers, with limited exceptions, to take the vaccine if they wanted to keep their jobs.
Another concern about forcing workers to get vaccinated is that it could prompt hesitant employees to resign. That’s a particular worry in long-term care, where the pandemic has exacerbated a shortage of certified nursing assistants.
“We’re having a hard time filling those roles and those positions now, and if we lose more people, then our old people are going to suffer,” said Dane Henning, Director of Public Affairs at the National Association of Health Care Assistants. … (read more)

10 Steps to Reform
and Improve Nursing Homes
Expert insights on how the industry should evolve in response to CO
Jan. 13, 2021 – AARP – by Sari Harrar, Joe Eaton and Harris Meyer

It’s complicated. This phrase has become the default and arguably lazy response to many 21st-century challenges. But when it comes to finding ways to reform and improve America’s nursing homes, it is sadly accurate.
The roots of the long-term care industry’s problems are deeply tangled, as we reported in the December issue of the AARP Bulletin.
…A nursing home aide can be responsible for more than 20 residents on a shift. The job is physically and emotionally demanding, and lives can be at stake, yet the average wage is around $13 an hour. Requirements for the job vary by state. In most, workers complete a hands-on training course and a certified nursing assistant (CNA) program, which generally take from 75 hours of training to more than three months. But don’t be fooled by the terminology. State requirements to gain a hairstylist license are more demanding than for a CNA, says Lori Porter, cofounder and CEO of the National Association of Health Care Assistants. Now that COVID-19 restrictions have limited CNAs to working at just one facility, many are unable to afford basic living expenses. … (read more)

Executive Outlook 2021: Nursing Home Stigma
Will Linger ‘for Some Time’ — for Both
Residents and Staff
Jan. 10, 2021 – Skilled Nursing News – by Alex Spanko
If there’s been one recurring theme for SNN’s annual executive outlook, it’s the idea that putting 2020 to bed represents a chance to reset and move on past the worst year in the history of the post-acute and long-term space, both in the United States and around the world.
But that can only happen if the public and the frontline workers who serve our seniors believe that change is possible — and forthcoming.
The stories of admission declines and vaccine hesitancy among caregivers prove that trust in nursing homes has never been lower, and that coming back from a world-historic disaster won’t be a simple matter of flipping over a calendar page.
Lori Porter, CEO, National Association of Health Care Assistants
I — along with many, many others — am happy to see the year 2021 and have 2020 in the rearview. The last year was incredibly difficult on everyone, especially those in our field. The pandemic has been on a rampage through America’s nursing homes, wreaking havoc on our elders. However, the new year signifies a new beginning, a fresh start, and new opportunities. New opportunities often come with new challenges.
As co-founder and CEO of the association of and for certified nursing assistants (CNAs), my focus is lasered in on the front line. What was once a generally safe profession is now one of the most dangerous in America due to the pandemic. … (read more)

Nursing Home COVID-19 Vaccine Rollout
Slow in Early Going, with 13% of
Shots Distributed
Jan. 5, 2021 – Skilled Nursing News – by Alex Spanko
Only about 13% of the first COVID-19 vaccine doses have been administered to nursing home residents by the first business week of 2021, raising concerns about the rollout for both the elderly and the general public.
The federal government’s long-term care vaccination initiative has about 3.3 million total doses set aside, but just 429,066 had been administered in the setting as of January 5, according to the most recent data from the Centers for Disease Control & Prevention (CDC); the latter figure represents just the first dose in the two-stage vaccination process. Around 17 million vaccine doses have been distributed nationwide, with about 4.8 million first rounds injected thus far, the CDC reported…
…Operators are also beginning to face predicted resistance to the vaccine among nursing home staff, who have spent the last 10 months on the front lines of a crisis that has shown no signs of abating. In Ohio, for instance, up to 60% of workers declined the vaccine, Gov. Mike DeWine indicated last week, despite more widespread acceptance among residents.
Lori Porter, CEO and co-founder of the National Association of Health Care Assistants, said last month that many of the certified nursing assistants (CNAs) that her organization represents have lost faith in institutions — including the government and their employers — after witnessing firsthand the COVID-19 disaster in long-term care.
“My concern is not necessarily the vaccine, if it’s proven safe,” Porter told SNN. “My fear is that if we don’t educate them, if we allow the facilities to provide the education on the vaccine, there is a trust issue. CNAs do not trust their leaders.” … (read more)

Shots are slow to reach arms as Trump administration
leaves final steps of mass vaccination to beleaguered states
Dec. 30, 2020 – Washington Post – by Isaac Stanley-Becker

In suburban Milwaukee, clinicians recently discarded 500 doses of coronavirus vaccine after vials were “intentionally” left unrefrigerated. In southeastern Arizona, a rural clinic has enough shots but too few employees lining up to take them. And on the coast of Maine, physicians have been left in the dark about when they will get vaccinated.
The largest immunization campaign in U.S. history is off to a slow start, dimming hopes, at the end of a dismal year, of an imminent return to normal.physicians have been left in the dark about when they will get vaccinated.
In some places, the vaccination campaign — among the most complex logistical efforts initiated in peacetime — has been marked by chaos and confusion. Many medical workers who believe they should have priority access are finding that inoculation remains elusive. And most states moved into the third week of immunization not yet beginning to get shots to long-term care facilities, which have been epicenters of infection……But hesitancy among nursing home staffers looms as a significant hurdle. Lori Porter, who leads the National Association of Health Care Assistants, said polling she has reviewed suggests a significant majority of people working in stricken facilities “are a hard no” on taking the vaccine. “Often, people have to see something before they can believe something, especially in this political climate,” she said, predicting at least moderate improvement as immunization becomes a reality across the country. … (read more)

Executive Outlook 2021: Nursing Home Stigma
Will Linger ‘for Some Time’ — for Both
Residents and Staff
Jan. 10, 2021 – Skilled Nursing News – by Alex Spanko
If there’s been one recurring theme for SNN’s annual executive outlook, it’s the idea that putting 2020 to bed represents a chance to reset and move on past the worst year in the history of the post-acute and long-term space, both in the United States and around the world.
But that can only happen if the public and the frontline workers who serve our seniors believe that change is possible — and forthcoming.
The stories of admission declines and vaccine hesitancy among caregivers prove that trust in nursing homes has never been lower, and that coming back from a world-historic disaster won’t be a simple matter of flipping over a calendar page.
Lori Porter, CEO, National Association of Health Care Assistants
I — along with many, many others — am happy to see the year 2021 and have 2020 in the rearview. The last year was incredibly difficult on everyone, especially those in our field. The pandemic has been on a rampage through America’s nursing homes, wreaking havoc on our elders. However, the new year signifies a new beginning, a fresh start, and new opportunities. New opportunities often come with new challenges.
As co-founder and CEO of the association of and for certified nursing assistants (CNAs), my focus is lasered in on the front line. What was once a generally safe profession is now one of the most dangerous in America due to the pandemic. … (read more)

Nursing Homes Grapple With Staff
Hesitant to Get the Covid-19 Vaccine
Dec. 22, 2020 – Skilled Nursing News – by Maggie Flynn
With two COVID-19 vaccines officially authorized for use, the immunization of health care workers and long-term care facility residents is finally underway in earnest. The Food and Drug Administration granted emergency use authorizations (EUAs) to Pfizer’s (NYSE: PFE) COVID-19 vaccine on December 11 and to Moderna’s (Nasdaq: MRNA) on December 18. There are several considerations for skilled nursing facilities to take into account as they prepare for the inoculations, from how to handle staff concerns about taking the vaccine to preparing for the impact side effects could have on scheduling.
Vaccinating staff is the critical first step for facilities, from which all the other considerations about workflow and coordination will spring. A webinar held on December 17 tackled some of those considerations. Hosted by the National Association of Health Care Assistants (NAHCA) and AMDA – The Society for Post-Acute and Long-Term Care Medicine, the virtual event gave an overview of some of the concerns expressed by certified nursing assistants (CNAs), with questions and answers between frontline staff and long-term care physicians.
Ultimately, long-term care workers will not be forced to take COVID-19 vaccines, webinar speakers said, even though an advisory committee for the CDC recommended that health care workers and long-term care residents be first in line. “I’m not going to get up here and tell you that ‘You have got to take the shot, get the vaccine,’” Lori Porter, the CEO and co-founder of NAHCA, said during the webinar. “That is a choice you will have to make yourself.” … (read more)

Vaccine Push at Nursing
Homes Meets Resistance
Dec. 17, 2020 – Barrons.com – by Eleanor Laise

Sherry Perry has seen all the horrors of the pandemic. As a certified nursing assistant at a long-term care facility in Lebanon, Tenn., she has held a phone up to a window so a daughter could say goodbye to her dying father. She has watched residents die alone, not understanding why their families didn’t visit them in their final days. Earlier this month, she herself got Covid, suffering fever and chills, and passing out as she struggled to breathe.
As the Covid-19 vaccine arrives in long-term care facilities this month, however, Perry, who is also a board member of the National Association of Health Care Assistants (NAHCA), says she and many of her co-workers are concerned about side effects and distrustful of the government.
As the Covid-19 vaccine arrives in long-term care facilities this month, however, Perry, who is also a board member of the National Association of Health Care Assistants (NAHCA), says she and many of her co-workers are concerned about side effects and distrustful of the government.With a maximum of six paid sick days a year, she fears having to take unpaid time off. Her facility hasn’t told staff anything about the vaccine’s arrival, she says, and “that throws people into panic mode,” because they fear they’ll be pushed into taking a brand-new vaccine that they don’t fully understand.. … (read more)

Vaccination Campaign at Nursing
Homes Faces Obstacles and Confusion
Dec. 16, 2020 – The New York Times – by Rebecca Robbins and Jessica Silver-Greenberg
It promises to be a crucial milestone in America’s battle against a pandemic that has inflicted especially severe carnage on nursing homes. At least 106,000 residents and staff of long-term care facilities have died from the virus, accounting for 38 percent of the country’s Covid-related fatalities.
But even before it begins, the mass-vaccination campaign is facing serious obstacles that are worrying nursing home executives, industry watchdogs, elder-care lawyers and medical experts. They expect nursing homes to be the most challenging front in the mission to vaccinate Americans…
…“I don’t want to be a guinea pig,” said Sheena Bumpas, a certified nursing assistant at a home in Duncan, Okla. She is far from alone. When the National Association of Health Care Assistants, an advocacy group for caregivers, recently surveyed certified nursing assistants who work in long-term care facilities, nearly 72 percent of respondents said they do not want to receive the vaccine.
Lori Porter, the group’s co-founder and chief executive, said employees are also worried about what happens if they experience side effects — some participants in clinical trials experienced mild to moderate side effects — that force them to stay home. Ms. Porter said many nursing assistants had to use sick days to quarantine earlier in the pandemic and now have little or no paid sick leave left for 2020. … (read more)

Who’s to Blame for the
100,000 COVID Dead in Long-Term Care?
Dec. 3, 2020 – AARP.org

To understand who or what is to blame for the more than 100,000 deaths caused by the coronavirus among residents and staff of U.S. long-term care facilities between March and Thanksgiving, it’s useful to consider a devastating calamity that hit in 2005: Hurricane Katrina.
In the days, weeks and months after New Orleans was overwhelmed with flooding from the hurricane, critics pointed to the slow response from the federal government, decisions made by the city’s mayor and the state’s governor, a delay in engagement from the U.S. president, the greed and influence of private businesses, and even the stubbornness of the city’s residents as the causes for all the pain that had occurred.
Some level of truth. But in time, two simple but profound causes were ultimately found to be the root of what happened: bad infrastructure decisions that dated back decades—in New Orleans’ case, a poorly maintained, inadequate levee system — and a storm of such magnitude that once 23 of the levees were breached, little could be done to prevent 80 percent of the city from going underwater…
…In July, a report published by the National Bureau of Economic Research raised alarms about the common practice of care staff working in multiple facilities. Nursing homes with higher rates of shared staffing, the researchers found, had higher rates of infection. Limiting care staff to a single nursing home, they concluded, could reduce COVID-19 infections in facilities by 44 percent.
That’s no surprise to Lori Porter, cofounder of the National Association of Health Care Assistants, which represents many nursing home care workers. With an average wage of around $13 an hour, care workers often work at multiple nursing homes to make ends meet, Porter says. Many staffers don’t receive health insurance or paid sick leave, leading some to work even when they were experiencing coronavirus-type symptoms. “What did you think was going to happen?” Porter says. … (read more)

If There’s No Trust, There’ll
Be More Hesitancy’:
Nursing Homes Must Overcome
Staff Skepticism of COVID Vaccine
Dec. 2, 2020 – Skilled Nursing News – by Maggie Flynn
The Centers for Disease Control and Prevention (CDC) was emphatic in a Tuesday meeting that it has the systems and processes in place to keep track of any adverse events from a COVID-19 vaccine, whenever one is approved.
Whether that is enough to quell the concerns of the health care workers and long-term care facility residents — whom the CDC’s Advisory Committee on Immunization Practices (ACIP) this week recommended should be first in line for immunization — is still an open question.
“There is hesitancy, of course,” Lori Porter, the CEO and co-founder of the National Association of Health Care Assistants (NAHCA), told Skilled Nursing News on December 2. “Until we know if it’s mandated or not, we’re not really going to know exactly what’s going to happen. From what we can tell, the CDC won’t make it mandatory. It’ll be up to the states, and the states might pass it off to the facilities as more of an employer policy. So until we know what the outcome is, there is a great deal of hesitancy among CNAs [certified nursing assistants].” … (read more)

Lori Porter – On Transforming
Working Conditions for CNAs
Oct. 18, 2020 – Senior Living Foresight – by Steve Moran

Hands-heartIn response to COVID-19 and the disastrous impact it has had on nursing homes, the president established an independent body called the Coronavirus Commission on Safety and Quality in Nursing Homes. One of the members of the commission was Lori Porter the CEO of the National Association of Health Care Assistants.
some level of truth. But in time, two simple but profound causes were ultimately found to be the root of what happened: bad infrastructure decisions that dated back decades—in New Orleans’ case, a poorly maintained, inadequate levee system — and a storm of such magnitude that once 23 of the levees were breached, little could be done to prevent 80 percent of the city from going underwater…
…In July, a report published by the National Bureau of Economic Research raised alarms about the common practice of care staff working in multiple facilities. Nursing homes with higher rates of shared staffing, the researchers found, had higher rates of infection. Limiting care staff to a single nursing home, they concluded, could reduce COVID-19 infections in facilities by 44 percent.
That’s no surprise to Lori Porter, cofounder of the National Association of Health Care Assistants, which represents many nursing home care workers. With an average wage of around $13 an hour, care workers often work at multiple nursing homes to make ends meet, Porter says. Many staffers don’t receive health insurance or paid sick leave, leading some to work even when they were experiencing coronavirus-type symptoms. “What did you think was going to happen?” Porter says. … (read more)